1601006153 : LONG CASE (GM Final Practical)
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.
Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
This E log book also reflects my patient-centered online learning portfolio and your valuable inputs on the comment box is welcome.
A 61 year old gentleman who is resident of Kangaal ,shepherd by occupation came with complaints of pain in abdomen from 10days,Fever from 2 days
HISTORY OF PRESENT ILLNESS:
Patient was apparently asymptomatic 10 days ago ,then he developed
1. Pain in abdomen
-from 10 days
-It is a diffuse type , insidious in onset , progressive, dragging associated with shortness of breath , it was non radiating pain with no diurnal variations , it was relieved by sleeping sideways
2.Fever
From 2 days ,Low grade ,continous associated with chills and rigor ,relieved on taking medication.
No History of Nausea, Vomitings , Loose stools, flatulence ,loss of weight decreased urine output, dysuria.
PAST HISTORY:
-He had yellowish discoloration of eyes 6 months ago.
- No history of diabetes mellitus, hypertension, tuberculosis, epilepsy.
PERSONAL HISTORY:
•Mixed diet
•Appetite adequate
•Bowel movements are irregular as he is constipated.
•Bladder movements are regular.
•He is a chronic alcoholic takes 90ml/day since 30 yrs
•He is a chronic smoker and takes 20 beedis/day since 30 yrs.
FAMILY HISTORY:
-Not significant
TREATMENT HISTORY:
Took medication in local hospital 6 months back for jaundice.
ON GENERAL EXAMINATION,
-The patient is conscious, coherent and cooperative.
- He is well oriented to time, place and person.
- He is moderately built and moderately nourished.
-Examination was done after taking proper consent & in a well lit room after adequate exposure.
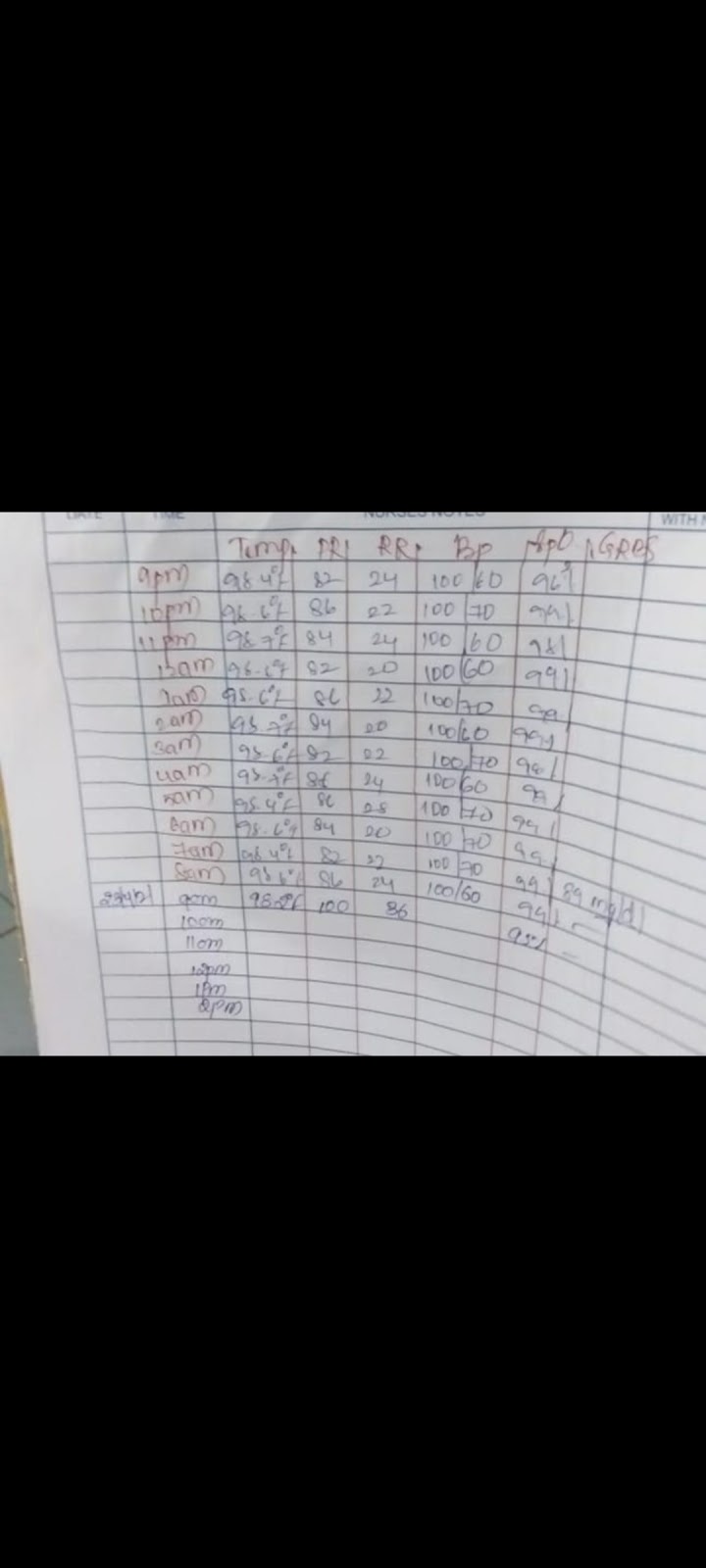
Vitals :
- Temperature = he is afebrile (at present)
Pulse = 84 beats per minute, regular, normal in volume and character. There is no radio-radial or radio-femoral delay. The condition of the arterial wall is normal.
- Blood pressure = 120/70 mm of Hg-
- Respiratory rate = 22 cycles per minute.
-Sp O2 :93% at room air
- JVP is normal
-Bulbar conjunctiva of left and right eye are yellow in color.
Bipedal edema ,pitting type, upto the level of ankle region
Local examination
Oral cavity : brown staining of teeth
GASTROINTESTINAL EXAMINATION :
On Inspection,
•Anterior abdominal wall
- Abdomen is symmetrically distended with full flanks
-Umblicus is below the midposition between xiphisternum and pubic symphysis, Slightly everted with horizontal Slit .
Abdomen skin is smooth and shiny
-All the quadrants are equally moving with respiration
-No venous prominence when examined both on sitting and standing position.
-No scars ,ulcers ,visible pulsations.
- No Scratch marks on the abdomen.
-No hernial swellings with and without cough impulse
• Posterior abdominal wall,
No scars , swellings, pulsations
On palpation
•Superficial palpation ,
- Localised tenderness in the right hypochondrium
- elastic consistency
- No rise in temperature,guarding and rigidity,thrills
•Deep palpation,
- Liver is tender ,smooth ,firm , regular margin, moving with respiration.
- Spleen , kidneys , urinary bladder are not palable
-Abdominal girth is 84 cms
On Percussion,
Liver span - 16 cms
No shifting dullness
On auscultation,
Bowel sounds are heard
No venous hum,bruit, friction rub.
RESPIRATORY EXAMINATION
Upper respiratory tract examination -
Nose: No deviated nasal septum, No nasal polyps
Pharynx : no post nasal drip , congestion
Inspection;
•Shape of Chest is symmetrical ,Elliptical
•Trachea appears to be Central (Trails sign -ve)
•Movements of chest equal on the both sides
•No Visible Pulsations, Swellings, Engroged Veins, Scars & Sinuses
•No signs of use of accessory muscles of respiration.
Palpation;
- No local rise of temperature
- Trachea Central
- Respiratory movements are normal
- Chest Expansion 5cm (from 80-85cm)
- Transverse diameter 29cm
-AP diameter 24cm
- Vocal fermitus Decreased on Right side lower region
- Apex beat is palpable in 5th intercoastal space ,1 cm medial to mid clavicular line
- No palpable lymph Nodes
Percussion;
Direct : resonant over clavicular, sternum.
Indirect :
Anterior. Right. Left.
Supraclavicular: Resonant. Resonant Infraclavicular: Resonant. Resonant
•Stony dull note on the right seventh intercostal space
• Resonant note in second to sixth right intercostal space
• Resonant note from second to sixth left intercostal space
Lateral chest wall
Dull note in the right InfraAxillary region
Posterior: Right Left.
Suprascapular: Resonant. Resonant
Interscapular: Resonant resonant
Infrascapular: Dull . Resonant
Auscultation:
Right. Left
•Supraclavicular. Normal. Normal
• Infraclavicular. Normal. Normal
• Mammary Normal. Normal
•InfraMammary. Decreased. Normal
• InfraAxillary. Decreased. Normal
• suprascapular. Normal. Normal
• Infra Scapular. Decreased Normal
• Interscapular. Normal. Normal
CVS
Normal S1 S2 heard
No murmurs
Apex beat felt on 5th intercostal space
No focal deficits seen
INVESTIGATIONS :
Complete blood picture
Liver function test
Ultrasound Abdomen
Aspiration of liver abcess
Pleural fluid examination
Pleural tap
Chest X-ray
ABDOMEN X-RAY
TREATMENT :-
1.INJ.MEROPENAM 500mg I.V ,BD
2.Inj.metrogyl 750mg I.V TID
3.Inj .pantop 40mg I.V,twice daily
4.Tab.Lasix 40 mg orally once daily
5 Tab.doxycycline 100mg oral twice daily
6.Tab.Linezoid 600mg per orally twice daily
7.Syrup lactulose 15 ml orally twice daily
8 Inj Vit.K 1 ampoule in 20ml .Normal saline I.V once daily
PROVISIONAL DIAGNOSIS :
Multiple pyogenic liver Abcess with right side pleural effusion.